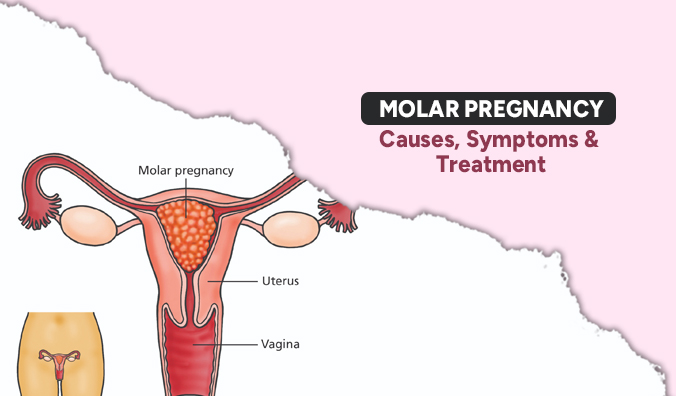
Molar pregnancies, occurring in just 0.1% of pregnancies, stem from abnormal placental development, leading to the formation of fluid-filled sacs or cysts in the uterus. This unconventional pregnancy is nonviable as the faulty placenta cannot adequately support fetal growth. While rare, it poses health risks for the mother. Women with a history of molar pregnancy are at higher risk and should remain vigilant for symptoms in subsequent pregnancies. Dr. Jeyarani Kamaraj, a best gynecologist for pregnancy care, offers exceptional expertise at Aakash Fertility Hospital, making her the top choice for expectant mothers seeking quality medical attention.
Causes of molar pregnancy
The exact causes of molar pregnancy remain unknown, suggesting it occurs randomly without any controllable factors for women. It can affect women across all ages, ethnicities, and backgrounds.
During fertilization in a molar pregnancy, an egg and sperm fuse incorrectly, leading to the formation of a noncancerous tumor. These tumors, resembling clusters of small water-filled sacs, lack the ability to support embryo development, resulting in pregnancy loss. While some women may experience miscarriage, others may require medical intervention for tumor removal. Untreated molar pregnancies can potentially lead to severe complications.
Symptoms of molar pregnancy
- Vaginal bleeding, often darker or more watery than usual
- Severe nausea and vomiting (hyperemesis gravidarum)
- Enlarged uterus that is disproportionate to the stage of pregnancy
- Rapid uterine growth
- High blood pressure (hypertension)
- Excessive thyroid function (hyperthyroidism)
- Symptoms of anemia, such as fatigue and weakness
- Passage of grape-like cysts or tissue through the vagina
- Pelvic pain or discomfort
It’s important to note that these symptoms can also be associated with normal pregnancies or other medical conditions, so if you experience any of these, it’s crucial to consult with a best gynecologist at Aakash fertility hospital for proper evaluation and diagnosis.
Treatment options for molar pregnancy
Evacuation of the abnormal tissue: The primary treatment for a molar pregnancy is the removal of the abnormal tissue from the uterus. This is usually done through a procedure called suction curettage, where a thin tube is inserted into the uterus to suction out the tissue.
Follow-up care: After the tissue is removed, close monitoring is necessary to ensure that all of the abnormal tissue has been successfully evacuated. This may involve regular blood tests to measure hormone levels and occasional imaging studies, such as ultrasound, to check for any remaining tissue.
Hormone therapy: In some cases, hormone therapy may be prescribed following the removal of the molar tissue to prevent the regrowth of abnormal cells and reduce the risk of complications.
Future pregnancy planning: After successful treatment, most women can go on to have healthy pregnancies in the future. However, close monitoring by a healthcare provider is usually recommended to ensure that there are no complications or recurrences in subsequent pregnancies.
At Aakash Hospital, top fertility clinic in Chennai, distinguished for its exceptional fertility care, you’ll find dedicated professionals ready to provide personalized support and a wide range of services. Take the first step towards realizing your fertility aspirations by reaching out to schedule an appointment today.