The initial step in assessing female fertility involves a comprehensive consultation with our fertility specialist at Aakash IVF hospital. During this session, a detailed exploration of your medical history and lifestyle is conducted. A comprehensive physical examination is also conducted and pelvic exam, including a pap smear, is integral to female fertility testing. Following the initial appointment, the gynecologist may recommend initial testing to assess factors such as ovulation patterns, ovarian function, and uterine function during the ovulation process.
Urine Test: Our fertility specialist Dr. Jeyarani Kamaraj may recommend a luteinizing hormone (LH) urine test. This test is effective in detecting the surge in LH concentration that occurs just before ovulation.
Blood Test: Depending on your medical history and the suspected diagnosis, the doctor will prescribe specific lab tests. These may include assessments for thyroid function, prolactin levels, ovarian reserve, and progesterone levels.To find IVF doctors near me for infertility blood tests, consider scheduling an appointment with Dr. Jeyarani Kamaraj and Dr. Niveditha Kamaraj. Their expertise and proximity make them convenient choices for personalized care on your journey for pregnancy.
Pap Smear Test: This examination aims to identify abnormal cells around the cervix, detecting sexually transmitted diseases and cervical irregularities, including the presence of cervical cancer. Any of these factors could potentially pose challenges to conception.
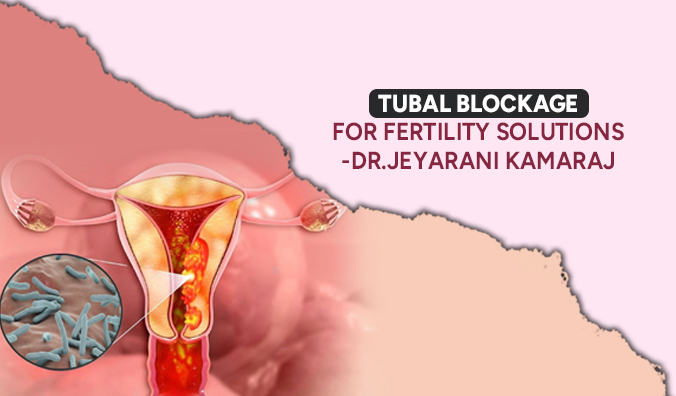
Hysterosalpingogram (HSG): Also referred to as a “tubogram,” this procedure involves taking multiple X-rays of the uterus and fallopian tubes. A liquid dye is introduced through the vagina to enable X-ray imaging. The HSG helps identify uterine issues or blocked fallopian tubes and is typically conducted shortly after menstruation.
Transvaginal Ultrasound: Using an ultrasound “wand” inserted into the vagina, this procedure examines pelvic organs. Sound waves are utilized to visualize the ovaries and uterus, facilitating the detection of any abnormalities.
Saline Sonohysterogram: This test assesses the uterine lining for polyps, fibroids, and structural irregularities. During a transvaginal ultrasound, saline (water) is injected into the uterus to expand it, providing a clearer view of the uterine cavity for the healthcare professional.
FSH Test: FSH levels are measured before and after taking the medication, specifically on day 3 and day 10. Elevated FSH levels may indicate reduced chances of pregnancy.
Laparoscopy: Through a few small abdominal incisions, instruments, including a camera, are inserted to examine the entire pelvis. This procedure allows for a comprehensive evaluation, addressing issues such as endometriosis affecting pelvic organs.
Hysteroscopy: This test involves inserting a flexible, thin instrument called a hysteroscope with a camera through the vagina and cervix. The device is advanced into the uterus to inspect the interior parts.
AMH Test: Additionally, gynecologists may recommend a blood test to assess anti-müllerian hormone (AMH) levels. The quantity of AMH offers insights into ovarian function, and very low levels may suggest a diminished ovarian reserve.
Endometrial Biopsy: An endometrial biopsy is a medical procedure in which a small sample of tissue is collected from the lining of the uterus, known as the endometrium. This biopsy is typically performed to investigate and diagnose various uterine conditions or concerns, such as abnormal bleeding, unexplained infertility, or to assess the endometrium’s response to hormonal treatments. The collected tissue is then examined under a microscope to provide insights into potential abnormalities or issues affecting the uterine lining.
Book your appointment at Aakash IVF Hospital Reproductive Clinic for specialized care in addressing female infertility. Our dedicated team of fertility experts will conduct a thorough evaluation of your medical history, utilizing advanced diagnostics to provide personalized solutions. Take the first step towards your fertility journey with the top IVF hospital in Chennai, Aakash IVF Hospital for compassionate and expert care.