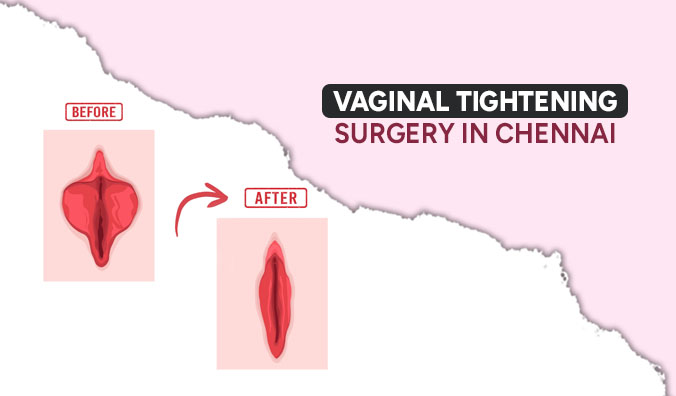
Vaginal tightening refers to procedures or techniques aimed at restoring or enhancing the tightness and tone of the vaginal muscles and tissues. This can be achieved through various methods, non-surgical treatments like laser therapy or radiofrequency devices, and surgical procedures like vaginoplasty or labiaplasty. The goal of vaginal tightening is often to improve sexual satisfaction, alleviate symptoms of vaginal laxity or incontinence, and enhance overall vaginal health and function. For Vaginal tightening procedure book your appointment with Dr. Niveditha Kamaraj, best cosmetic gynecologist, Aakash hospital in Chennai.
Who needs Vaginal Tightening surgery?
- Childbirth: After giving birth, some women experience vaginal laxity or looseness due to stretching of the vaginal tissues during delivery. Vaginal tightening surgery can help restore the pre-pregnancy tightness.
- Aging: As women age, hormonal changes, such as a decrease in estrogen levels, can lead to vaginal atrophy, thinning of vaginal walls, and decreased elasticity, resulting in vaginal laxity. Vaginal tightening surgery can help address these changes.
- Improved Confidence: Some individuals may feel self-conscious or insecure about the appearance or feel of their genitals due to vaginal laxity, leading them to opt for vaginal tightening surgery to boost their confidence and self-esteem.
- Urinary Incontinence: Vaginal laxity can sometimes contribute to urinary incontinence, and tightening the vaginal muscles through surgery may help alleviate this issue.
- Desire for Rejuvenation: Like other cosmetic procedures, some people opt for vaginal tightening surgery as a means of rejuvenating and enhancing their genital area.
What happens during Vaginal Tightening surgery?
During vaginal tightening surgery, excess vaginal tissue is removed, and the vaginal muscles are tightened and reshaped to improve tone and elasticity. The cosmetic gynecologist sutures the incisions to secure the tightened tissues in place. Following the procedure, patients may experience some discomfort, swelling, and bruising, which can be managed with medication and ice packs. Post-operative instructions are provided for proper hygiene and activity restrictions. Follow-up appointments are scheduled to monitor healing progress and address any concerns.
Benefits offered by Vaginal Tightening Surgery:
- Enhanced Intimacy: Restoring vaginal tightness can improve intimacy and closeness between partners, fostering a stronger emotional connection.
- Correction of Vaginal Laxity: Vaginal laxity, which can result from childbirth or aging, can be corrected through surgery, helping women regain confidence in their vaginal tone and appearance.
- Alleviation of Urinary Incontinence: In some cases, vaginal tightening surgery can help reduce symptoms of urinary incontinence by strengthening the pelvic floor muscles, which support the bladder.
- Increased Confidence and Self-Esteem: Addressing concerns about vaginal laxity can boost self-confidence and self-esteem, leading to an overall improvement in quality of life.
- Rejuvenation: Vaginal tightening surgery can provide a rejuvenating effect on the genital area, helping individuals feel more youthful and vital.
- Correction of Physical Discomfort: Some women may experience physical discomfort or irritation due to vaginal laxity, which can be alleviated through surgery.
- Restoration of Pre-Pregnancy Vaginal Tone: For women who have given birth, vaginal tightening surgery can restore the vaginal tone and tightness experienced before childbirth.
What outcomes are possible with Vaginal Tightening treatments?
A woman will feel more comfortable during strenuous or sexual activities after this procedure. Vaginoplasty can tighten the vagina and bring it back to the same size as it was before childbirth. Overall, this will increase the woman’s self-confidence.
To undergo a vaginal tightening procedure, make an appointment with Dr. Niveditha Kamaraj, a top cosmetic gynecologist, at Aakash Hospital in Chennai.